I remember the day when I finally received my diagnosis after being misdiagnosed for 8 years and wondering “what is the best diet for Hashimoto’s?”
Like you, I was concerned about what I would be able to eat and it seemed life was going to be difficult where food was concerned.
At the time, I could not imagine how eliminating gluten and dairy was going to be enjoyable. I did finally get past that stage and today I enjoy a world of delicious foods in a variety of combinations that I never knew existed. Giving up gluten (including gluten in cosmetics, especially lipstick & lipgloss) was really a no-brainer for me because I understood the science behind it.
The havoc gluten wreaks on the body and brain over time just wasn’t worth it. Dairy, on the other hand, was a major challenge…I loved the taste of milk and Gouda cheese was my favorite of all cheeses. But, with the commitment, I did give up dairy and I’ve never looked back. I will share an interesting tidbit with you. After I gave up both gluten and dairy, my doctor and I were both amazed at one particular lab result, and it wasn’t my TPO antibodies. I had a huge shift in my eGFR, or “estimated glomerular filtration rate.” This is an assessment of kidney function. My eGFR prior to changing my diet wasn’t good for my age, it was in the low 70s. Just to give you an idea, a value of 60 or less should raise a red flag with your doctor as this it may be an indicator of declining kidney function. After eliminating gluten and dairy my eGFR jumped to 119! And I’ve seen the same amazing result happen for many of my clients. Kidney health is just another great reason to give up gluten and dairy.
What foods are we supposed to eat?
The autoimmune, thyroid and Hashimoto’s communities-at-large are usually advised to follow either a Paleo or Autoimmune Paleo (AIP) diet in an effort to reduce symptoms and antibodies and this is okay to a certain extent. The truth is there are “many shades” of Hashimoto’s and autoimmune disease, and for me, as a nurse-nutritionist and Hashimoto’s patient, there simply isn’t enough scientific evidence to prove that everyone with Hashimoto’s should be following one popular master diet long-term.
We are all unique and what may be good for me may not be good for you and so on. There are commonalities for sure and we all should be avoiding the top inflammatory foods such as gluten, grains, dairy, GMO-corn, soy protein, sugar, yeast, trans-fats, and certain cooking oils (cottonseed, soybean, safflower, corn, grapeseed, and sunflower.)
However, we need to take it a step further to make sure we are meeting our individual health needs. At one point in my own Hashimoto’s journey, I saw first-hand how true it really is in that food is either nourishing, healing and life-sustaining or it is potentially toxic and may even play a role in the progression of the disease process overall.
We live in a toxic world and even though, for example, asparagus is known to be a healthy food; for one individual it may be fine and yet result in triggering inflammation in another. This is because our immune systems don’t respond to foods in the exact same way. Factors like toxins, environment, stress and genetics play a role too.
So, the short answer to “what foods are we supposed to eat?” is highly individual.
A Major Problem with the Autoimmune Paleo Diet
One problem I see on a routine basis is significant nutrient deficiencies in my clients who follow AIP long-term. It’s sad because they believe they’re doing the “right thing” based on a popular book they’ve read or found on a website. It’s also sad because most of the nutrients they are found to be deficient are the nutrients required at the cellular level for energy. The typical scenario is the belief their symptoms of fatigue stem from incorrect thyroid dosage. In my own anecdotal research with clients, I have found their symptoms of fatigue and lack of energy is related to multiple nutrient deficiencies associated with the AIP diet.
The typical scenario is the client believes their symptoms of fatigue stem from incorrect thyroid dosage. In my own anecdotal research with clients, I have found their symptoms of fatigue and lack of energy is instead related to multiple nutrient deficiencies associated with the AIP diet. Their micronutrient lab results absolutely (I use SpectraCell) correlate with their symptoms. The good news is that following a replenishing protocol is helpful and effective for them.
I do believe AIP may prove helpful in the short term to help reduce inflammation and in making adjustments to learning to avoid certain foods and establishing new dietary habits as previously stated.
But seriously, are you really never going to enjoy a tomato, eggplant or other nightshades again for the rest of your life? If this is your plan, then you need to be prepared to take a boat load of supplements on a daily basis forever.
The key is learning the language of your own body through subjective AND objective testing and learn which foods cause inflammation for YOU, and those that do not.
Nutrient Deficiencies Commonly Associated with AIP
- Vitamin A
Signs of Deficiency: Bitot’s spots, color-blindness, conjunctivitis, dry, hard eyeballs, infected, ulcerating eyes, macular degeneration, night blindness, retinal detachment, sensitive eyes, photophobia, acne, dry skin, fish-like scales (skin), impetigo, cold sores, jaundice, scleroderma, shingles, warts, moles, dry hair, peeling nails, ridges on nails, - Vitamin B1 (Thiamine)
Signs of Deficiency: Dim vision, fatigue, adrenal exhaustion, Raynaud’s disease/syndrome, gangrene, sensitivity to insect bites, furrowed tongue, beriberi (a constellation of symptoms that affect the heart, nerves, and digestive system.), edema, confusion, congestive heart failure, enlarged heart, peripheral neuropathy, macular atrophy, nerve pain, muscle tenderness, fast heart rate. - Vitamin B2 (Riboflavin)
Signs of Deficiency: Blurred vision, cataracts, conjunctivitis, dim vision, retinitis, itching, burning, water, sandy eyes; macular degeneration, night blindness, red blood vessels in the sclera, retinal detachment, photophobia, tics of eyelids, acne, adrenal exhaustion, eczema, skin ulcers, seborrhea, oily skin, whiteheads, purplish or blue-black skin areas, rosacea, scaly eczema around nose, ears, vulva or scrotum in males; vaginal itching, dandruff, oily hair, burning/sore tongue, cracked lips & corners of mouth, distended, purplish-blue veins under the tongue, white patches on tongue, purplish or magenta tongue or lips, also veins under the tongue. - Vitamin B3 (Niacin)
Signs of Deficiency: Pellagra, red-brown, often symmetrical discoloration of skin exposed to the sun, later ulceration, mouth ulcers, canker; papillae prominent or erased, red tongue at tip or edges, severe: whole tongue scarlet red & sore; tongue too small or too large; diarrhea, mental disorders, dermatitis. - Vitamin B5 (Pantothenic Acid)
Signs of Deficiency: Retinitis, adrenal exhaustion, Addison’s disease, graying hair, beefy, enlarged tongue; vitiligo, furrowed tongue, tongue too small or too large, - Vitamin B6 (Pyridoxine)
Signs of Deficiency: Blurred vision, fatigue, peripheral neuropathy, nerve pain, dark spots in front of the eyes, retinitis, infected, ulcerating eyes; macular degeneration, night blindness, retinal detachment, tics of eyelids, acne, adrenal exhaustion, eczema, skin ulcers, edema, Raynaud’s disease/syndrome, oily dermatitis around eyes or nose, painful red skin on pressure areas (e.g. knees, elbows), infections on the skin (boils, cold sores, impetigo, etc), itching, jaundice, over-sensitivity to sunlight, skin cancer, stretch-marks, fluid retention, swellings (face, lower extremities), dandruff, opaque nails, white spots/bands on nails, burning sore tongue, cracked lips & corners of the mouth, halitosis (bad breath). - Vitamin B7 (Biotin)
Signs of Deficiency: Acne, graying hair, hair loss, pale skin, scaly dermatitis, loss of appetite, brittle nails, inflammation of the eye, inflammation of the skin, brittle hair, low immunity, depression, lethargy, lack of concentration, fatigue, shortness of breath, heart failure, irregular ECG, fungal infections. - Vitamin B9 (Folate/Folic Acid)
Signs of Deficiency: Feeling weak or tired, lightheaded, irritability, loss of appetite, inability to concentrate, graying hair, cracked lips & corners of the mouth, pale skin, mouth ulcers, canker sores, - Vitamin B12 (Cobalamin)
Signs of Deficiency: Fatigue, weakness, pale skin, a smooth tongue, retinitis, brown discoloration around small joints, jaundice, lemon-yellow skin, shingles, swellings (face), constipation, loss of appetite, diarrhea, vision disturbance, depression, loss of memory, numbness or tingling, muscle weakness, heart palpitations, shortness of breath. - Vitamin D
Signs of Deficiency: Near-sightedness, rickets, cancer, bone pain, muscle weakness, cardiovascular disease, autoimmune disease. - Calcium, Copper, Chromium, Iron, Magnesium, Phosphorus, Selenium, Zinc
Food Sensitivity Issues & Testing
More than 2,000 years ago the Roman poet and philosopher, Lucretius said: “what is food to one man may be bitter poison to others.” Now more than ever, diet plays a critical role in preventing a wide range of degenerative diseases and premature aging.
The key is learning which foods (in addition to the standards we know to avoid) may cause even low-level inflammation in your body.
I used to advocate for the elimination diet and I don’t believe in that anymore…not for people like you and me who have Hashimoto’s or other thyroid or autoimmune illnesses. Why guess? Why take chances? Nobody knows what their cells are doing at the molecular level and not all inflammatory responses in the immune system produce obvious symptoms of any kind; however, that does not mean they’re not adding to the progression autoimmunity.
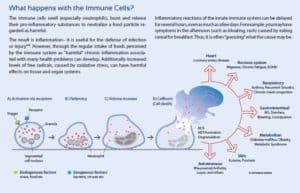
My point is you don’t need to guess at it when there are scientifically proven methods to find out. The immune system is a double-edged sword. It should react appropriately and protect against infection when confronted with harmful invaders or “infectious agents” like viruses or bacteria.
Unfortunately, for many people with Hashimoto’s or other autoimmune diseases, exposure to common foods, chemicals, molds, and herbs, may trigger chronic activation of the immune system. There is a lot of debate about whether we should be testing IgG antibodies or not. The facts regarding food specific antibody testing lead to the conclusion that many commercial claims of laboratories are misleading. For example:
Elevated levels of IgG antibodies to foods DO NOT mean that a hidden or delayed reaction to food is detected.
Food-specific IgG antibody levels DO NOT necessarily correlate with chronic symptoms.
IgG antibodies DO NOT cause inflammation or a leaky gut.
IgG blood tests DO NOT detect Type III hypersensitivities.
Diets based on IgG levels to foods HAVE NOT BEEN SHOWN to successfully diminish symptoms.
Yale University stands behind this methodology as does Baylor Medical College and other institutions. Just because your body may produce an IgG antibody against broccoli, for example, does not mean that the IgG antibody is contributing to your symptoms in any way whatsoever. IgG antibodies and TPO antibodies originate from different pathways in the immune system.
I have worked with hundreds of clients and have found the Alcat Test to be more effective than standard IgG tests because IgG testing relies exclusively on one immune pathway only: serum levels of IgG. Having high food-specific IgG titers is indicative only of exposure, not necessarily intolerance. Therefore, high frequency of consumption or overexposure may lead to false positives. I’ve provided an excellent research article (with citations) for you below. You may also share it with your practitioner if he or she is still using IgG testing for food sensitivities.
Food Sensitivity Testing_Alcat vs IgG antibodies – A Scientific Review
If you would like to learn more about the ALCAT Food & Chemical Sensitivity Test, you may visit our dedicated Food Sensitivity Testing page for details.
Please remember this Hashi’s Sister, the best diet for YOU is a diet which avoids those foods that trigger inflammation in your immune cells. A food sensitivity is not something you would necessarily be aware of because there may not be obvious symptoms. When the white blood cells are exposed to a food or chemical that causes the cell to rupture or change shape is really what’s going on in food intolerance/sensitivity issues. So, it is very important to test every couple of years or so – because your test results SHOULD change if you’re healing your gut and reducing inflammation. Also, be sure to avoid those foods that are known to be associated with molecular mimicry and/or suppress thyroid function: gluten, dairy, GMO-corn, and soy protein.
Take a look at the image below to understand what actually happens to the cell when it is exposed to a certain food or chemical it is intolerant/sensitive to:
I hope you found this article helpful. If you’re doing everything right (that you’ve learned online, etc) and you still feel fatigued, it may be time to look at food & chemical sensitivity and micronutrient testing and implementation of an individualized diet and nutrient replenishing protocol ASAP so you can feel better.