True to many people’s experience, the bowel can be extremely sensitive to stress. In the condition which is known as irritable bowel syndrome (IBS), stressors disrupt the digestive tract’s rhythmic contractions, which is why this syndrome has also been called, descriptively, spastic colon.
Because of these irregular contractions, food and waste do not move through the system normally, and the intestine becomes partially blocked. Resulting symptoms, which tend to be chronic; include sensations of fullness, gas, bloating and cramping; diarrhea and constipation which often alternate.
Physical exams usually reveal no particular sources for the discomfort; it is generally accepted that emotional conflicts and tension must be among the primary triggering stressors. An unbalanced diet, food sensitivities, food allergies and eating too fast may also be the trigger for symptoms.
Managing stress and dealing with emotional issues are the first steps are the first steps in bringing bowel function back to normal again. Evaluating diet, altering eating patterns and correcting any nutritional deficiencies are equally important.
I remember my late teens/early 20s when I was supporting myself and living on my own, I experienced symptoms similar to IBS. Back then, my doctors diagnosis was “spastic colon” and he prescribed (according to memory) a medication called Combid Spanules. It was in capsule form and I remember the clear capsules filled with tiny yellow “beads.” I kept the bottle in my purse at all times due to the fear and anxiety of being in public and having an “emergency” and embarrassing myself. I’m sure my symptoms were due to emotional stress and anxiety related to living on my own at such a young age and trying to navigate the world in general. I can’t help but wonder if what I was going through then with my health was somehow the foundation for autoimmune disease 12 years later. If only I knew then what I know now…
IBS Symptoms and Diagnosis
Miscellaneous Conditions Associated with IBS
- Stress & anxiety
- Depression
- Fibromyalgia
- Chronic fatigue syndrome
- Chronic pelvic pain
- Low back pain
- Temporomandibular joint dysfunction (TMJ)
- Various gynecological disorders
- Interstitial cystitis
- Headaches
- Insomnia
- Overactive bladder
Autoimmune Diseases that Overlap with IBS
- Addison’s disease
- Autoimmune lymphoproliferative syndrome
- Celiac disease
- Dermatomyositis
- Graves disease
- Hashimoto’s thyroiditis
- Inflammatory Bowel Disease
- Multiple Sclerosis
- Myasthenia gravis
- Pernicious anemia
- Psoriasis
- Rheumatoid arthritis
- Scleroderma
- Sjögren syndrome
- Systemic Lupus Erythematosus
- Type I diabetes
Although there is no test that definitively confirms a diagnosis of IBS, subjective assessment criteria have been established in order to assist doctors in making a diagnosis of IBS.
Manning (1978) and Rome (I, II, III, IV) criteria. Manning criteria were originally introduced in 1978 as a symptom-based questionnaire and included what were thought to be classic IBS-symptom related questions. Today, Manning criteria are no longer viewed as being reliable since it doesn’t help practitioners in making the distinction between IBS with constipation (IBS-C) and IBS with diarrhea (IBS-D). Rome IV (2016) is the most recent criteria useful for research and clinically as an aid to diagnosis rather than an absolute. Prior to Rome IV, doctors utilized Rome I (1992), Rome II (1999) and Rome III (2006) as assessment tools to aid in the diagnosis of IBS.
According to Rome IV criteria, IBS is defined as:
a functional bowel disorder in which recurrent abdominal pain is associated with defecation or a change in bowel habits. Disordered bowel habits are typically present (i.e., constipation, diarrhea or a mix of constipation and diarrhea), as are symptoms of abdominal bloating/distension. Symptom onset should occur at least 6 months prior to diagnosis and symptoms should be present during the last 3 months.
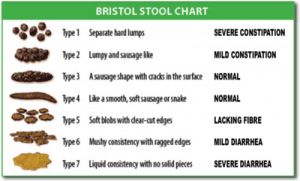
The Bristol Stool Form Scale (1990) is also a subjective test, relies on “stool types” to aid in the assessment and determination of an IBS diagnosis. It was developed in the Bristol Royal Infirmary in England for the assessment of stool. The authors classified stool into 7 “types” with clear descriptions and determined which types may be associated with IBS-constipation and IBS-diarrhea. See below:
What You Can Do
First, you must see a physician to rule out conditions such as diverticulitis, Crohn’s disease, or gastroparesis. If no organic cause is found for your symptoms, assess your eating habits, including your food choices and eating behaviors: when you eat, how often, how fast, size of meals and tension levels during meals. Note which foods your bowel is especially sensitive to; dairy products, cabbage, and legumes are often culprits. Avoid rich foods, eat small, regular meals and eat slowly.
Calm Your Mind & Body
Find quiet and private time each day when you can slow your pace and recenter yourself. Even a few minutes can make a difference. Regular practice of relaxation techniques such as deep breathing, stretching, infrared sauna, meditation, walking, and restorative yoga is even better for calming your mind, muscles and internal organs. Acupuncture has also been helpful for people with IBS. Antianxiety herbs can also make a difference. Try valerian, St. John’s wort, oats, oats straw, kava kava, and skullcap to help settle your mind and your intestine.
Apply Heat to Relieve Pain
Applying heat to the abdomen and back may relieve sharp pain or dull aching by relaxing the cramped intestinal muscles. Heating pads, hot wet towels, and hot water bottles will all do an effective job soothing tense muscles.
Drink Peppermint Tea to Soothe Spasms
Research has shown peppermint to be especially helpful for irritable bowels. Drink peppermint tea every day to relax cramping, alleviate bloating, and soothe the intestinal lining.
First Aid Remedy
Caraway helps relieve cramps and is an excellent first aid for bloating and gas related stomach pain. Take 8 drops of caraway oil in a glass of hot water. You can also chew a few caraway seeds or drink caraway tea: Boil 1 tablespoon of caraway seeds in 1 cup of water for 5 minutes and strain.

- Veggie enteric-coated capsule; Gluten-free; No soy or soybean oil; Safflower oil as an emulsifier
- A novel safe long-term therapy for the management of IBS symptoms. Symptoms include diarrhea, constipation, spasms, gas or bloating and burping.
- Fixed combination of peppermint/caraway oil clinically tested with an overall effective rate of 95% for patients with IBS in just 4 weeks.
- Clinically tested for IBS
- The overall effective rate of 95% – IBS
- Recommendation for IBS: 1 capsule, 3 times daily, to relax spastic bowel and wall muscle
Nutritional Remedies
If you suffer from a chronically sluggish bowel, try taking 1-2 tablespoons of whole flaxseed each day with plenty of water or mixed into gluten-free oatmeal or cream of brown rice cereal. In the intestines, the seeds exude a gummy substance that absorbs water and swells, which encourages intestinal function. You can also take 2 tablespoons of flaxseed oil directly or use it in salad dressings. Flaxseed oil has been shown to help increase short-chain fatty acids and reduce inflammation. In addition to Regimint:
- Digestive enzymes 5 minutes before the beginning of each meal to diminish excess gas and bloating caused by diminished bowel flora that produces these enzymes. Look for a digestive enzyme product that contains artichoke, black radish, and other digestive aids.
- L-glutamine taken with each meal will help to rejuvenate the mucosal lining of the bowel associated with inflammation.
- EPA fish oil capsules with each meal to decrease inflammation in the bowel.
- Probiotics and prebiotics to restore and replenish beneficial gut flora.
- To prevent constipation, cut out all white flour and dairy products; they are not easily digestible. Soluble fiber in the form of psyllium guar gum with each meal may help. In general, increase your fiber intake with vegetables and fruits. Always drink plenty of water.
- To combat diarrhea, grate an unpeeled apple and eat or serve as soon as it turns brown.
- Avoid intestinal irritants such as coffee, sodas, very spicy or acidic foods and food additives and preservatives.
- Although a low FODMAPS diet is the standard recommendation for people with IBS, it’s not effective for everyone. Dietary recommendations should be customized and dependent on each individual’s needs according to their food sensitivity/intolerance and food allergy issues. We recommend the ALCAT test for anyone with digestive issues, autoimmune disease, and IBS.
Medicinal Teas
For acute constipation, try laxative teas made from buckthorn bark, rhubarb, aloe or senna leaf. To prevent too harsh a laxative action, blend these herbs with mint, caraway, or ginger. Use these teas for not more than a few days.
For diarrhea, try chamomile tea.
For bloating, try teas with peppermint, caraway, fennel and/or aniseed.
For feelings of fullness try mugwort, wormwood, or bitter-orange-peel teas.
For tension and nervous excitement, try teas with calming herbs, such as hops, lemon balm, valerian or passionflower.
Flower Remedies
Flower remedies may relieve IBS symptoms through their harmonizing influence on the psyche. One of these remedies might be right for your state of mind. Take 4 drops 4 times daily, 10 minutes before meals.
- Rockrose for panic and fear
- Beech for hypercritical attitude
- Impatiens for impatience, irritability, and a tendency to overreact
Recommended Resources
- The IBS Network
- The Quick and Easy IBS Relief Cookbook
- Irritable Bowel Syndrome.net
- Mega Sporebiotic – (patient code: microbiome)
Mega Sporebiotic plays a unique role in the regulation of the microbiome including the species which play a role in constipation and diarrhea. Additional therpaeutic benefits of Mega Sporebiotic include the following:- Aids in digestion
- Improves regularity
- Helps control bacterial overgrowth
- Detoxifies the intestinal tract
- Reduces inflammation & pain
- Assists in the reduction of cholesterol
- Produces key nutrients – antioxidants (via HU36™), B-vitamins, Vitamin K2, Nattokinase, and CoQ10
- Provides immune modulation for the prevention and treatment of infections, allergies and asthma
- Download your copy of the starter nursing care plan and nutrition support protocol:
We value your privacy and would never spam you
References
- https://www.ncbi.nlm.nih.gov/pubmed/8268145
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5704116/
- https://en.wikipedia.org/wiki/Bristol_stool_scale
- https://www.ncbi.nlm.nih.gov/pubmed/24100754
- https://irritablebowelsyndrome.net/clinical/is-ibs-an-autoimmune-disorder/
- Segala, M. (Ed.). (2003). Irritable Bowel Syndrome. The Life Extension Foundations disease prevention and treatment protocols, 1998: Offshore medical therapies, natural alternatives to toxic drugs, therapies for “untreatable” diseases, based on thousands of research studies(4th ed.). Hollywood, FL: Life Extension Media.



Leave A Response